Abstract
Background: In response to inflammation, neutrophils expel NETs, decondensed chromatin coated with histones and granular proteins that capture pathogens. NET degradation products (NDPs), including cell free (cf) DNA, citrullinated histone 3 (citH3), and myeloperoxidase (MPO), are elevated in adults with COVID-19 and contribute to endothelial injury. However, NETs have not yet been quantified in pediatric patients with active SARS-CoV-2 infection, or children who develop the post-infection inflammatory syndrome MIS-C. Although NDPs can be measured in plasma samples in the research setting, it has been proposed that smudge cells (SC), leukocyte remnants composed of extracellular chromatin that are identified by automated digital morphology systems, represent circulating NETs. Automated quantification of SCs is attractive strategy to quantify systemic NET load because it is routinely performed on patient samples as part of a standardized clinical laboratory evaluation.
Aims: The aims of this study are to measure NETs in the plasma of children with COVID-19 or MIS-C, and to determine if NDP and SC% elevation correlate with NET levels
Methods: We analyzed plasma samples obtained from patients admitted to The Children's Hospital of Philadelphia (CHOP) with COVID-19 between April and October 2020, including children with mild (N=21) or severe (N=13) COVID-19, and MIS-C (N=23). Remnant plasma from healthy patients (N=13) was used as a control. Samples were analyzed with the Olink Explore 1536/384 protein biomarker platform, cfDNA was meauasred with a fluorescent plate assay, and citH3 was quantified wit a commercial ELISA (Cayman). Spearman rank correlation was used to quantify the association between cfDNA and citH3, protein biomarkers, and clinical data. We next reviewed 56 peripheral smears from patients with mild COVID-19(N=5), severe COVID-19 (N=8), and MIS-C (N=6), using the Cellavision® hematology autoanalyzer. Results were validated independently by two blinded observers, and Spearman rank correlation was used to measure the association between SC%, leukocyte counts, and clinical laboratory data.
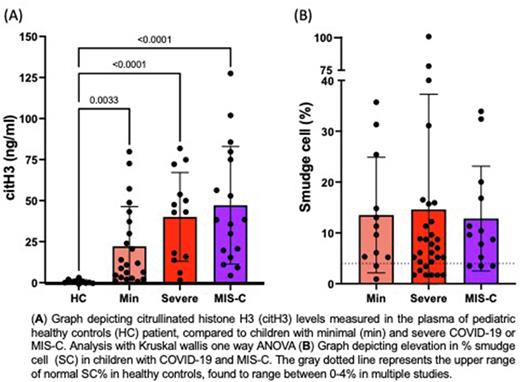
Results: cfDNA and citH3 were significantly elevated in pediatric patients with COVID-19 compared to healthy controls, with the highest levels observed in patients with severe COVID-19 and MIS-C (Figure 1). Correlative analysis with results of proteomic studies showed that citH3 was significantly associated with multiple markers of neutrophil activation including MPO, matrix metalloproteinase-9, and IL-8, demonstrating that citH3 is a specific marker of NET release. Although cfDNA does not exclusively originate from NETs, it was significantly correlated with the specific NET marker citH3 (r=0.7844, p<0.0001), suggesting that cfDNA is in part derived from NETs. Analysis of clinical data showed that citH3 was inversely correlated with sodium (r=-0.4289, p=0.011) and positive correlated with troponin levels (r=0.3587, p=0.0438). cfDNA significantly correlated with the complement membrane attack complex (r=0.2986, p=0.024) and LDH (r=0.5463, p=0.0015).
Review of peripheral smears showed SC levels were elevated in pediatric patients with COVID-19 (Figure 2). SC% positively correlated with monocytes (r=0.4047, p=0.0018) and eosinophils (r=0.3420, p=0.0092) and inversely correlated with neutrophil counts (r=-0.4064, p=0.0017), suggesting that many SC originate from neutrophils. SC% was also inversely correlated with activated partial thromboplastin time (aPTT,r=-0.5153, p=0.04), a finding that may indicate activation of the contact coagulation pathway by increased plasma NETs.
Conclusion: Plasma NET markers are elevated in the plasma of pediatric patients with COVID-19, with the highest levels observed in those with severe disease and MIS-C. Correlation of cfDNA and citH3 with proteins associated with neutrophil activation, complement fixation, and organ dysfunction adds support to our hypothesis that these markers originate from NETs and contribute to endothelial injury. SC% is elevated in children with COVID-19 infection and MIS-C. Further studies are underway to determine whether SCs originate from NETs. This work suggests there may be clinical utility in quantifying and reporting SC% in the hematology laboratory to identify increased NETs in children, a finding relevant to the study and treatment of COVID-19 and other viral infections.
Disclosures
Teachey:Sobi: Consultancy; BEAM Therapeutics: Consultancy. Bassiri:Kriya Therapeutics: Consultancy. Lambert:Octapharma: Membership on an entity's Board of Directors or advisory committees, Research Funding; Dova: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Principia: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Shionogi: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Research Funding; Argenx: Consultancy, Research Funding; Rigel: Consultancy, Research Funding; Sobi: Consultancy; Janssen: Consultancy; Sysmex: Research Funding; Astra Zeneca: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.